

Blood Types
- Share via Email
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
Facts About Blood and Blood Types
How blood type is determined and why you need to know.
Blood types are determined by the presence or absence of certain antigens – substances that can trigger an immune response if they are foreign to the body. Since some antigens can trigger a patient's immune system to attack the transfused blood, safe blood transfusions depend on careful blood typing and cross-matching. Do you know what blood type is safe for you if you need a transfusion?
Discover what blood types are compatible with yours.
Get our guide to find out..
There are four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells. In addition to the A and B antigens, there is a protein called the Rh factor, which can be either present (+) or absent (–), creating the 8 most common blood types ( A+, A- , B+, B- , O+, O- , AB+, AB- ).
Blood Types and Transfusion
There are very specific ways in which blood types must be matched for a safe transfusion. The right blood transfusion can mean the difference between life and death. Use the interactive graphic below to learn more about matching blood types for transfusions.
Also, Rh-negative blood is given to Rh-negative patients, and Rh-positive or Rh-negative blood may be given to Rh-positive patients. The rules for plasma are the reverse.
- The universal red cell donor has Type O negative blood.
- The universal plasma donor has Type AB blood.
There are more than 600 other known antigens, the presence or absence of which creates "rare blood types." Certain blood types are unique to specific ethnic or racial groups. That’s why an African-American blood donation may be the best hope for the needs of patients with sickle cell disease , many of whom are of African descent. Learn about blood and diversity.
What Is A Universal Blood Donor?
Universal donors are those with an O negative blood type. Why? O negative blood can be used in transfusions for any blood type.
Type O is routinely in short supply and in high demand by hospitals – both because it is the most common blood type and because type O negative blood is the universal blood type needed for emergency transfusions and for immune deficient infants.
Approximately 45 percent of Caucasians are type O (positive or negative), but 51 percent of African-Americans and 57 percent of Hispanics are type O. Minority and diverse populations, therefore, play a critical role in meeting the constant need for blood.
Types O negative and O positive are in high demand. Only 7% of the population are O negative. However, the need for O negative blood is the highest because it is used most often during emergencies. The need for O+ is high because it is the most frequently occurring blood type (37% of the population).
The universal red cell donor has Type O negative blood. The universal plasma donor has Type AB blood. For more about plasma donation, visit the plasma donation facts.
Nearly 16 million blood components are transfused each year in the U.S." What is your blood type? Donate and find out.
What Is A Rare Blood Type?
There are more than 600 other known antigens, the presence or absence of which creates " rare blood types ." Your blood type is considered rare if you lack antigens that 99% of the people are positive for. If you somehow lack an antigen that 99.99% are positive for, your blood type is extremely rare.
How Is My Blood Type Determined?
It’s inherited. Like eye color, blood type is passed genetically from your parents. Whether your blood group is type A, B, AB or O is based on the blood types of your mother and father.

* Note: If you have questions about paternity testing or about blood group inheritance, your primary care physician should be able to provide you with an appropriate referral. Testing difficulties can cause exceptions to the above patterns. ABO blood typing is not sufficient to prove or disprove paternity or maternity.

Ready to Help Save a Life?
Now that you know how your blood type can help recipients, please schedule an appointment to donate today.

- Science Notes Posts
- Contact Science Notes
- Todd Helmenstine Biography
- Anne Helmenstine Biography
- Free Printable Periodic Tables (PDF and PNG)
- Periodic Table Wallpapers
- Interactive Periodic Table
- Periodic Table Posters
- Science Experiments for Kids
- How to Grow Crystals
- Chemistry Projects
- Fire and Flames Projects
- Holiday Science
- Chemistry Problems With Answers
- Physics Problems
- Unit Conversion Example Problems
- Chemistry Worksheets
- Biology Worksheets
- Periodic Table Worksheets
- Physical Science Worksheets
- Science Lab Worksheets
- My Amazon Books
Blood Types – A, B, AB, O, Rh

Blood types are a classification of blood based on the presence or absence of specific antigens on the surface of red blood cells. These antigens determine the body’s immune response to foreign substances and are crucial in the context of blood transfusions, organ transplants, and pregnancy.
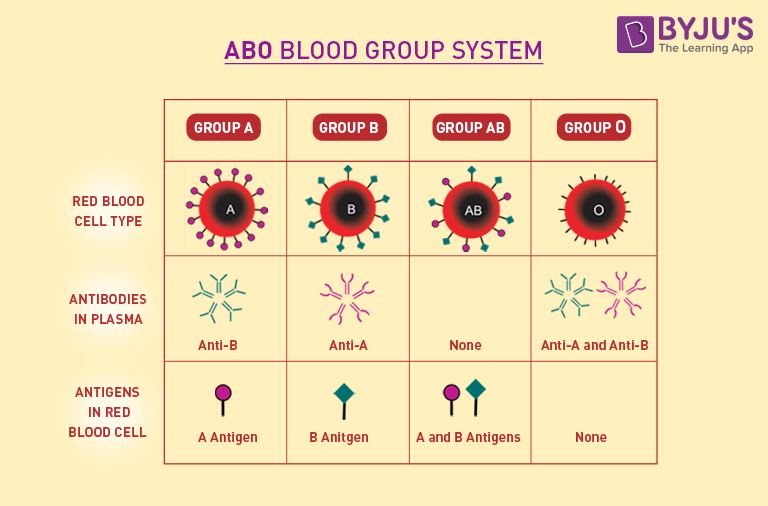
The ABO Blood Group System
The ABO blood group system is the primary blood type classification system. It categorizes blood into four main types:
- Type A: Has A antigens on the red cells and anti-B antibodies in the plasma.
- Type B: Has B antigens with anti-A antibodies in the plasma.
- Type AB: Has both A and B antigens, but no anti-A or anti-B antibodies. Known as the universal recipient.
- Type O: Has no A or B antigens, but both anti-A and anti-B antibodies. Known as the universal donor.
The Rh Factor
The Rh factor is another critical component of blood typing. It refers to the presence or absence of the Rh antigen, commonly known as the D antigen. Blood is either Rh-positive (Rh+) or Rh-negative (Rh-).
All Possible Blood Types
Combining the ABO system with the Rh factor, there are eight main blood types:
Rarest and Most Common Blood Types
The rarity of blood types varies depending on where you live. In the US:
- Rarest Blood Type: AB-, followed by B- and A-.
- Most Common Blood Type: O+, followed by A+ and B+.
Universal Donor and Receiver
- Universal Donor: O- (can be given to almost anyone, especially in emergencies).
- Universal Receiver: AB+ (can receive from all blood types).
Blood Transfusion Compatibility
- A can receive A and O
- B can receive B and O
- AB can receive A, B, AB, and O (universal recipient)
- O can receive only O (universal donor)
- Note: “Yes” indicates compatibility for a transfusion between the donor and recipient blood types.
Regarding the Rh factor, Rh+ can receive both Rh+ and Rh- blood, whereas Rh- can only receive Rh- blood.
Blood Types and Plasma Donation
The rules for plasma donation and transfusion are different from those for red blood cell transfusion because plasma contains antibodies, not antigens. Here’s how it works based on the ABO and Rh blood groups:
- AB Plasma: Universal plasma donor.
- O Plasma: Best for O recipients.
- A Plasma: Suitable for A and AB recipients.
- B Plasma: Suitable for B and AB recipients.
- T ype AB Plasma: Individuals with AB blood type are universal plasma donors because their plasma does not contain anti-A or anti-B antibodies. This means their plasma works for any recipient, regardless of the recipient’s blood type (AB, A, B, or O).
- Type O Plasma: Type O individuals, while universal red blood cell donors, are not universal plasma donors. Their plasma contains both anti-A and anti-B antibodies, which attack the red blood cells of recipients with A, B, or AB blood types. Therefore, type O plasma is only given to O recipients.
- Type A Plasma: Type A plasma can be given to recipients with type A and AB blood types, as it contains anti-B antibodies but not anti-A antibodies.
- Type B Plasma: Type B Plasma can be given to recipients with type B and AB blood types, as it contains anti-A antibodies but not anti-B antibodies.
The Rh factor (positive or negative) is less critical in plasma transfusions compared to red blood cell transfusions. This is because plasma does not typically contain Rh antibodies unless the donor has been sensitized (e.g., a woman with Rh-negative blood type who has been pregnant with an Rh-positive baby). However, in practice, compatibility is still considered to reduce any risk of reaction.
Blood Type Inheritance
Blood type inheritance is determined by the ABO and Rh genes inherited from parents. Each parent contributes one ABO allele and one Rh allele to their child.
Examples of Blood Type Inheritance
For example, if a parent has blood type A (AO genotype) and the other B (BO genotype), their child could have one of the following blood types: A (AO), B (BO), AB (AB), or O (OO). But, if one parent has blood type A (AA genotype) and the other parent has type B (BB) genotype, the blood type of a child is always AB.
Rh inheritance is separate from ABO inheritance. The Rh+ is dominant to the Rh- gene. So, an Rh+ parent has either two copies of the Rh+ gene or one, while the Rh- parent always has two copies of the Rh- gene. If one or both parents has two copies of the Rh+ gene, all children are Rh+ (even if the other parent is Rh-). Parents who are Rh- have Rh- children. If one parent has one Rh+ and one Rh- gene and the other parent is Rh-, there is a 50:50 chance for a child to be Rh+ or Rh-.
The phenotype of a person’s blood type is A, B, AB, O, Rh+, Rh- (an observable characteristic), while the genotype (e.g., AO, AB, BB) usually is unknown unless they have children or undergo genetic testing.
Rh Incompatibility and Pregnancy
Blood types play a significant role in pregnancy, primarily due to the potential for Rh incompatibility between the mother and the fetus. This occurs when an Rh-negative mother carries an Rh-positive baby. The mother’s body may recognize the baby’s Rh-positive red blood cells as foreign and produce antibodies against them. This is not usually a problem during a first pregnancy but can become an issue in subsequent pregnancies.
How Rh Incompatibility Affects Pregnancy
- Sensitization: If an Rh-negative mother is sensitized (i.e., her immune system has developed antibodies against Rh-positive blood), these antibodies cross the placenta and attack the red blood cells of an Rh-positive fetus in future pregnancies.
- Hemolytic Disease of the Newborn (HDN): This condition occurs when the mother’s antibodies destroy the fetus’s red blood cells, leading to anemia, jaundice, heart failure, and even fetal death in severe cases.
Preventing Rh Incompatibility Issues
- Rho(D) Immune Globulin (RhoGAM): Giving this medication to Rh-negative mothers during and after their first pregnancy with an Rh-positive baby prevents the mother’s immune system from becoming sensitized to Rh-positive blood cells. This protects future pregnancies.
ABO Blood Group and Pregnancy
While less common and usually less severe than Rh incompatibility, ABO incompatibility can also occur during pregnancy. This happens when the mother and baby have different ABO blood types, leading to the mother producing antibodies against the baby’s blood type. However, these antibodies are usually IgM, which do not cross the placenta, thus posing less risk to the fetus compared to the Rh incompatibility scenario.
Other Blood Type Systems
In addition to the well-known ABO and Rh blood group systems, there are several other blood group systems recognized by the International Society of Blood Transfusion (ISBT). These systems feature different sets of antigens on the surface of red blood cells. Some notable examples include:
- MNS System: This system depends on the presence or absence of M, N, S, s, and U antigens.
- Kell System: The Kell system includes antigens that are highly immunogenic, meaning they have a high potential to provoke an immune response. The most significant antigen in this system is the K antigen (also known as Kell or K1), and individuals are either K positive (K+) or K negative (K-).
- Duffy System: The Duffy system is associated with malaria resistance. The Duffy antigens (Fya and Fyb) play a role in how red blood cells interact with the parasites that cause malaria. People lacking these antigens (Fy-) are more resistant to certain types of malaria.
- Kidd System: The Kidd blood group system includes the Jka and Jkb antigens. Antibodies to these antigens cause transfusion reactions and hemolytic disease of the newborn.
- Lewis System: The Lewis blood group system is unique because Lewis antigens are not integral to the red blood cell membrane but are adsorbed onto the cell surface from plasma. Lewis antigens are involved in the body’s response to infections and are used in forensic testing.
- P System: This system includes several antigens, with the most prominent being P1. The presence or absence of these antigens is important in transfusion medicine.
- Lutheran System: The Lutheran blood group system features a large number of antigens, with Lua and Lub being the most significant. Antibodies to these antigens can cause transfusion reactions.
- Diego System: This system is important in certain populations, such as those of East Asian or Native American descent. The most notable antigens in this system are Dia and Dib.

Blood Types and Transplants
Blood groups are an important factor in organ transplants, much like in blood transfusions, but the considerations for transplantation are more complex. The compatibility of blood types between the donor and recipient is crucial for reducing the risk of transplant rejection. However, matching blood types is just one aspect of a multifaceted process. Here’s a closer look:
Blood Type Matching in Transplants
Blood groups matter in transplants, but maybe not in the way you expect:
- ABO Compatibility: Just as in blood transfusions, the ABO blood group system is critical in organ transplantation. An incompatible blood group potentially leads to immediate rejection of the transplanted organ.
- Rh Factor: Unlike in blood transfusions, the Rh factor is not a major concern in organ transplants.
Waiting Times for Transplants and Blood Groups
- Variability in Waiting Times: Some blood groups might wait longer for organ transplants due to the availability of compatible organs. For instance, Type O individuals can only receive organs from Type O donors, potentially leading to longer waiting times.
- AB Blood Group: Individuals with AB blood type often have shorter waiting times for certain transplants like kidney transplants because they can accept organs from any ABO blood group.
Beyond Blood Type Matching
Instead of matching blood groups, transplants require more comprehensive tests as well as aftercare.
- Tissue Typing (HLA Matching): Human leukocyte antigens (HLA) are proteins on the surface of cells responsible for the immune system’s recognition of self versus non-self. A closer HLA match between donor and recipient reduces the risk of organ rejection.
- Crossmatching: Before a transplant, a crossmatch test is done to ensure that the recipient’s body does not have pre-formed antibodies against the donor’s antigens, which could cause immediate organ rejection.
- Immunosuppression: Even with a good match, recipients typically need to take immunosuppressive medications for the rest of their lives to prevent rejection.
Can Your Blood Type Change?
Generally, a person’s blood type depends on genetics, so it remains constant throughout their life. However, there are very rare instances and specific medical conditions or interventions that change an individual’s blood type:
- Bone Marrow Transplant/Stem Cell Transplant: This is the most common situation where a change in blood type can occur. If a person receives a bone marrow transplant from a donor with a different blood type, the recipient’s blood type eventually changes to match the donor’s. This is because the blood cells are produced by the stem cells from the donor’s bone marrow.
- Certain Diseases or Infections: For example, there are cases where systemic lupus erythematosus (SLE) causes a temporary change in blood group, possibly due to autoantibody production.
- Blood Transfusions: In extremely rare cases and usually only in large volume transfusions, the blood type changes temporarily. This is not a true change in blood type but rather a mixing of donor and recipient blood.
- Chimerism: This rare condition occurs when an individual has two different sets of DNA, which happens as a result of a bone marrow transplant, a blood transfusion, or naturally in the case of certain types of twins. In some cases of chimerism, different parts of the body exhibit different blood types.
- Mutations: Very rare genetic mutations lead to changes in the antigens present on the surface of red blood cells, potentially altering the perceived blood type. However, such cases are extremely uncommon.
- Avent, N.D. (2009). “Large-scale blood group genotyping: clinical implications”. Br J Haematol . 144 (1): 3–13. doi :10.1111/j.1365-2141.2008.07285.x
- Fauci, Anthony S.; Braunwald, Eugene; et al. (1998). Harrison’s Principals of Internal Medicine . McGraw-Hill. ISBN 0-07-020291-5.
- Kremer Hovinga, I.; Koopmans, M.; et al. (2007). “Change in blood group in systemic lupus erythematosus”. Lancet . 369 (9557): 186–7, author reply 187. doi: 10.1016/S0140-6736(07)60099-3
- Maton, Anthea; Hopkins, Jean; et al. (1998). Human Biology and Health . Englewood Cliffs NJ: Prentice Hall. ISBN 0-13-981176-1.
- Stayboldt, C.; Rearden, A.; Lane, T.A. (1987). “B antigen acquired by normal A1 red cells exposed to a patient’s serum”. Transfusion . 27 (1): 41–4. doi: 10.1046/j.1537-2995.1987.27187121471.x
Related Posts
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Blood Types: What Letters, Positive, and Negative Signs Mean
What to Know About Your Blood Type
- Blood Types
- Why to Know Your Type
- Compatibility
- Significance in Pregnancy
- Finding Your Blood Type
Your blood type is a combination of letters and signs identifying antigens present or absent on the surface of your red blood cells. Antigens are substances that can trigger the immune system to produce antibodies. Antibodies are proteins that lead an attack on substances perceived as foreign "invaders."
Blood typing is essential if you need to receive a blood transfusion . Your antibodies can attack transfused red blood cells of incompatible types. Mixing certain blood types can have dangerous health consequences. Some types of blood are more common than others, and they vary in compatibility.
This article will discuss how blood types are identified, how rare or common they are, and what that means for you.
Illustration by Lara Antal for Verywell Health
How Many Blood Types Are There?
The ABO system has four major blood types: A, B, AB, and O. Blood types are further categorized by the presence (positive or +) or absence (negative or -) of the Rh(D) antigen on the surface of their red blood cells, also known as the Rh factor . This produces the eight major blood types.
A and B antigens are sugars. The type of sugar antigens a person has determines whether they have A, B, or a mix of A and B (AB). If they lack both A and B, they are type O.
Protein antigens identify if you have a negative or positive Rh factor. A plus (+) or minus (-) sign indicates the presence or absence of the Rh factor. The plus indicates the presence of the antigen, while the minus means it is not widely present. About 85% of the population is Rh positive.
The International Society of Blood Transfusion further divides blood types into blood group systems by other types of antigens that may be present. They have identified 45 different blood group systems with hundreds of different antigens.
Some blood types are found in a limited number of people. In the United States, the blood types each found in less than 5% of the population are:
- AB- : 0.6% of the population
- B- : 1.5% of the population
- AB+ : 3.4% of the population
Most Common
More than 70% of the people in the United States have one of these two common blood types:
- O+ : 37.4% of the population
- A+ : 35.7% of the population
What Is Golden Blood?
Golden blood is the rarest known type of blood in the world. It has no Rh antigens at all, known as Rh null . It is dubbed "golden blood" because it can be donated to people with almost any Rh blood type, including those with rare types of Rh antigens.
However, if people with golden blood need blood, they can only receive the same type of blood. Experts estimate that only about 50 people are known to have golden blood, which was first detected in Australian aboriginal people.
Reasons to Know Your Blood Type
If you need blood during surgery or due to an injury or illness, it's essential to receive blood of a type that is compatible with your own. The hospital laboratory will type your blood and match it to donor units to ensure you only receive compatible blood.
Otherwise, you may have a hemolytic transfusion reaction when your immune system detects foreign proteins on the cells of an incompatible blood type and attempts to destroy them. Transfusion reactions range from mild to life-threatening. They can appear right after a transfusion or up to weeks later.
You can also help others by knowing your blood type in case you are in a position to donate to another individual in need or because blood bank supplies of your type of blood are low.
Different blood types also appear to make people more or less likely to develop certain conditions, including kidney stones, high blood pressure during pregnancy, and bleeding disorders. One study found people with blood group A have a higher likelihood of infection with COVID-19 than those in blood group O.
Compatibility of Different Blood Types
Compatible blood types are based on whether the recipient has antibodies to the donor blood antigens or may develop them.
Early in life, your immune system forms antibodies against A or B antigens not present on your red blood cells. People with blood type A will have anti-B antibodies, and those with type B blood will have anti-A antibodies. Type O blood has both anti-A and anti-B antibodies. Type AB blood has neither A nor B antibodies.
Antibodies only form against the Rh factor if an Rh negative person is exposed to Rh positive blood due to transfusion or pregnancy. The following chart shows what types of blood are compatible with each other.
Universal Donors and Recipients
Type O negative blood is called a universal donor , meaning that it can be safely given to people with most other blood types and has a low risk of a transfusion reaction. People with type AB positive blood are known as universal recipients, meaning they can be given almost any type of blood safely.
Unless blood is needed immediately to save a person's life, the hospital laboratory will type the person's blood and perform compatibility testing with the donor blood units (crossmatching) to ensure the safety of the transfusion.
Testing Blood Types in Pregnancy
If you are pregnant, it's important to identify your Rh blood type so you and your healthcare providers can prevent the consequences of Rh incompatibility. This affects only pregnant people who are Rh negative.
If the pregnant person is Rh negative and the other parent is Rh positive, the fetus may be Rh positive. This is called Rh incompatibility.
This incompatibility will not affect a child born during a first incompatible pregnancy. During birth, however, the blood of the pregnant person and fetus mixes. The Rh negative pregnant person can develop antibodies to the Rh factor.
Those antibodies could harm subsequent fetuses that are Rh positive. The pregnant person's anti-Rh(D) antibodies will identify fetal Rh proteins as foreign and attack them. Fetal red blood cells can swell and tear in response, known as hemolytic disease of the fetus and newborn .
This can lower the fetus's or newborn's red blood cell count and lead to serious consequences, such as brain damage, pregnancy loss, or death of the newborn.
An Rh negative pregnant person who has not developed anti-Rh(D) antibodies should given RhoGAM, or intravenous WinRho, a Rho(D) immune globulin to prevent the development of the antibodies.
How to Find Out Your Blood Type
A blood test can determine your blood type . If you donate blood or plasma , blood typing will be performed at no charge. You can learn your blood type from the report of the donor service.
Blood typing is not a part of routine blood tests. It's commonly ordered if you are having surgery, need a blood transfusion or organ transplant, or are pregnant.
You could request a blood type test from your healthcare provider, but it may not be covered by health insurance if it isn't medically necessary. At a healthcare facility, a small amount of blood will be drawn and sent to a lab for testing.
Check your medical record to see if a blood type test was done in the past and is reported there. If you are unsure how to access your medical record, ask your healthcare provider.
Home blood type tests are available in most states. They are generally accurate if performed correctly. Saliva tests are another option, but they may be more costly and less accurate.
While your blood type doesn't change, a blood type test will be performed each time you need a transfusion. An incompatible transfusion can be fatal, so extreme care is taken to ensure you receive only compatible units.
Blood typing is reported using the ABO blood system and the presence or absence of the Rh(D) antigen known as the Rh factor, resulting in eight major blood types. Some blood types are much more common than others.
If someone needs a blood transfusion, it is essential to use the same or a compatible type of blood to avoid potentially serious reactions to a transfusion. Pregnant people and their healthcare providers must know their Rh factor status to avoid hemolytic disease of the fetus and newborn.
Professional laboratory blood typing is more reliable than home tests, though home blood type tests are available.
Stanford Blood Center. Blood types.
International Society of Blood Transfusion. Red cell immunogenetics and blood group terminology.
Stanford Blood Center. Blood types .
Australian Academy of Science. Rare blood types .
MedlinePlus. Hemolytic transfusion reaction.
Dahlén T, Clements M, Zhao J, Olsson ML, Edgren G. An agnostic study of associations between ABO and RhD blood group and phenome-wide disease risk . Ginsburg D, Wittkopp PJ, Desch KC, eds. eLife. 2021;10:e65658. doi:10.7554/eLife.65658.
Wu SC, Arthur CM, Jan HM, et al. Blood group A enhances SARS-CoV-2 Infection . Blood . 2023;142(8):742-747. doi:10.1182/blood.2022018903
National Library of Medicine. The ABO blood group.
American College of Obstetricians and Gynecologists. The Rh factor: how it can affect your pregnancy.
Myle AK, Al-Khattabi GH. Hemolytic disease of the newborn: a review of current trends and prospects . Pediatric Health Med Ther. 2021;12:491-498. doi:10.2147/PHMT.S327032
Eldon Biologicals A/S. Eldoncard: home blood type testing kit .
Velani PR, Shah P, Lakade L. Determination of ABO blood groups and Rh typing from dry salivary samples. Int J Clin Pediatr Dent . 2018;11(2):100-104. doi:10.5005/jp-journals-10005-1493
By Nancy LeBrun LeBrun is a Maryland-based freelance writer and award-winning documentary producer with a bachelor's degree in communications.
- Biology Article
- Blood Groups
Blood Groups-ABO Blood Group and Rh Group System
Blood is a fluid connective tissue and the most crucial component of the circulatory system. In a healthy person, approximately 5 liters (12 pints) of blood circulates throughout their body. In this article, blood groups and their types are explained in detail.

Composition of blood is rather interesting. It consists of erythrocytes, leukocytes and platelets suspended in plasma along with the millions of different molecules with its own specific roles and functions.

Even though components of blood are the same for all humans, there are various blood types. In fact, there are more than 40 blood groups, but all of them are not clinically significant. The discovery of the ABO blood group created great excitement as until then, all blood had been assumed to be the same.
Blood Group System
Karl Landsteiner, an Austrian scientist discovered the ABO blood group system in the year 1900. In his experiments, he mixed different blood types and noted that the plasma from certain blood type produced agglutinates or formed clusters which were caused by the absence of molecules on red blood cells and resulting in antibodies to defeat that molecule. He then made a note of the agglutination and divided the blood types into 4 different groups. For the discovery of ABO blood group, he was awarded the Nobel Prize.
The blood grouping system is pivotal in blood transfusion. Our immune system recognizes another blood type as foreign and attacks it if introduced in the body causing a transfusion reaction . Any inappropriate match with the Rh and ABO blood types, causes the most serious and life-threatening transfusion reactions. Therefore, before blood transfusion, it is suggested to have a blood group checked.
What are ABO and Rh blood groups?
During the blood transfusion, the two most important group systems examined are the ABO-system and the Rhesus system .
The ABO blood group system consists of 4 types of blood group – A, B, AB, and O and is mainly based on the antigens and antibodies on red blood cells and in the plasma. Both antigens and antibodies are protein molecules in which antigens are present on the surface of Red Blood Cells and antibodies are present in the plasma which is involved in defending mechanisms.
On the other hand, the Rh blood group system consists of 50 defined blood group antigens. In the Rh system, the most important antigens are D, C, c, E, and e. The ABO and Rh blood systems are discussed in detail below.
1. ABO blood Group system
The basis of ABO grouping is of two antigens- Antigen A and Antigen B. The ABO grouping system is classified into four types based on the presence or absence of antigens on the red blood cells surface and plasma antibodies.
- Group A – contains antigen A and antibody B.
- Group B –contains antigen B and antibody A.
- Group AB –contains both A and B antigen and no antibodies (neither A nor B).
- Group O – contains neither A nor B antigen and both antibodies A and B.
The ABO group system is important during blood donation or blood transfusion as mismatching of blood group can lead to clumping of red blood cells with various disorders. It is important for the blood cells to match while transfusing i.e. donor-recipient compatibility is necessary. For example, a person of blood group A can receive blood either from group A or O as there are no antibodies for A and O in blood group A.
As shown in the above table, individuals of blood group O are called as universal donors , whereas individuals of blood group AB are universal recipients .
2. Rh Blood Group System
In addition to the ABO blood grouping system, the other prominent one is the Rh blood group system. About two-thirds of the population contains the third antigen on the surface of their red blood cells known as Rh factor or Rh antigen ; this decides whether the blood group is positive or negative. If the Rh factor is present, an individual is rhesus positive (Rh+ve); if an Rh factor is absent individual is rhesus negative (Rh-ve) as they produce Rh antibodies. Therefore, compatibility between donor and individual is crucial in this case as well.
Frequently Asked Questions
What are blood group antigens and antibodies.
The ABO system divides blood into four major blood groups:
- Blood type A contains anti-B antibodies and A antigens in the plasma.
- Blood group B contains anti-A antibodies and B antigens in the plasma.
- Blood type O has both anti-A and anti-B antibodies in the plasma but no antigens.
- Blood type AB lacks antibodies but possesses both A and B antigens.
How are blood antibodies formed?
The immune system uses antibodies white blood cells produce to recognise and combat foreign elements in the body. Red blood cells have blood type antigens on their surface, but the immune system does not recognise them. However, antibodies will recognise the antigens of a different blood type as foreign and attack them.
To learn more about Blood groups with interactive video lessons, keep visiting BYJU’S.
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Explore BYJU’S for more concepts on Biology
Your result is as below
Request OTP on Voice Call
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
Very helpful thanks Byju’s
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.

IMAGES
COMMENTS
Download Guide. There are four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells. In addition to the A and B antigens, there is a protein called the Rh factor, which can be either present (+) or absent (–), creating the 8 most common blood types (A+, A-, B+, B-, O+, O-, AB+, AB-).
Essay On Blood Types. 714 Words3 Pages. Our blood type plays a huge role in our body along with our nutrition and lifestyle. As we all know, there are 4 different blood types: A, B, AB, O. we cannot affect our blood type in any way later on in life since it forms while we are still in the womb. Every single blood type has its own ...
The ABO blood group system is the primary blood type classification system. It categorizes blood into four main types: Type A: Has A antigens on the red cells and anti-B antibodies in the plasma. Type B: Has B antigens with anti-A antibodies in the plasma. Type AB: Has both A and B antigens, but no anti-A or anti-B antibodies.
Also learn about the importance of blood group studies. Essay # 1. A, B and O Groups: i. The phenomenon of haemoagglutination is due to the interaction between two factors-agglutinogens, present in the corpuscles and agglutinins, present in the plasma (or serum). ii. There are two primary agglutinogens—A and B; and there are two corresponding ...
The ABO system has four major blood types: A, B, AB, and O. Blood types are further categorized by the presence (positive or +) or absence (negative or -) of the Rh (D) antigen on the surface of their red blood cells, also known as the Rh factor. This produces the eight major blood types. A and B antigens are sugars.
The difference in blood types was discovered in the 1900s. Blood transfusions can only be completed after matching blood types. Everyone does not carry the same blood type although blood type O is the most common in the United States (US). The four blood types we know of are type A, B, O and AB. The ABO blood type is determined genetically.
In the Rh system, the most important antigens are D, C, c, E, and e. The ABO and Rh blood systems are discussed in detail below. 1. ABO blood Group system. The basis of ABO grouping is of two antigens- Antigen A and Antigen B. The ABO grouping system is classified into four types based on the presence or absence of antigens on the red blood ...
Blood group, classification of blood based on inherited differences in antigens on the surfaces of the red blood cells. The most well-known classification, the ABO blood group system, was developed by Austrian-born American biologist Karl Landsteiner in 1901. Learn more about blood groups in this article.
ABO blood group system, the classification of human blood based on the inherited properties of red blood cells (erythrocytes) as determined by the presence or absence of the antigens A and B, which are carried on the surface of the red cells. Persons may thus have type A, type B, type O, or type AB blood. The A, B, and O blood groups were first ...
The type of antigen on the surface of your red blood cells determines your blood type. There are four basic blood types, made up from combinations of the type A and type B antigens. Type A: The red blood cells have the type A agglutinogen. Type B: The red blood cells have the type B agglutinogen. Type AB: The red blood cells have both type A ...