Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.

Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is a gay male, not currently sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound
- TheFreeDictionary
- Word / Article
- Starts with
- Free toolbar & extensions
- Word of the Day
- Free content
- presentation
pre·sen·ta·tion
Patient discussion about presentation.
Q. What are the presenting signs of ALS? Are the upper or lower extremeties affected initialilly? A. The most common presenting sign of ALS is asymmetric limb weakness, usually starting with the hands (problems with pinching, writing, holding things etc.) shoulders (lifting arms above head etc.) or legs (problems walking). Other presenting signs may be problems with speaking or swallowing, although these are less common. You may read more here: www.nlm.nih.gov/medlineplus/amyotrophiclateralsclerosis.html
Q. Iam a bipolar and presently on tegretol medication.I found this to be the best way to get my doubt clarified. I am a bipolar and presently on tegretol medication. My doctor frequently changes the meds and he has tried variety of medicines before prescribing tegretol. He changes the meds every time when I visit him for routine check-up. I am bit confused and obviously cannot question my doctor as I repose faith and confidence in him. I found this to be the best way to get my doubt clarified. A. Are you being treated by your GP? I would suggest if you are having trouble finding the right combinations it might be a good time to ask to be referred to a Psychaitrist. GP's will do their best but like anything specialized they only have a certain amount of knowledge and a specialist in the field could be more help. I also think that other treatments along with The medications like theropy and group theropy, excercise, good diet, plenty of sleep etc helps a lot too... Try to be patient it is a process to get everything in place that will work the best for you... everyone is different and the .mmedications and treatments that work for one may not work for another...
- 21-hydroxylase deficiency
- abnormal presentation
- anterior presentation
- antigen presentation
- asynclitism
- atypical GERD
- bacterial meningitis
- bipolar version
- presbyosmia
- prescapular fossa
- prescribed experience
- prescribing
- prescribing nurse
- prescription
- prescription drug
- prescription exemption certificate
- Prescription Medicines Code of Practice Authority
- prescription only medicine
- Prescription Pre-payment Certificate
- Prescription Pricing Authority
- Prescription Pricing Division
- presence of mind
- presenile dementia
- presenile spontaneous gangrene
- presenility
- presentative
- Presenteeism
- presenting symptom
- preseptal cellulitis
- preservation
- preservative
- presinusoidal
- presomite embryo
- presphenoid
- presphenoid bone
- presphygmic
- presplenic fold
- prespondylolisthesis
- pressed juice
- pressor base
- pressor fiber
- pressor fibers
- pressor nerve
- pressoreceptive
- Present Worth
- Present Worth of Capital Expenditures
- present you as
- present you with
- present yourself
- Present, The
- present-day
- Present-Day English
- Present-Minded Individualism
- present-worth factor
- presentability
- presentable
- presentablely
- presentableness
- presentably
- Presentance Report
- Presentaneous
- Presentasi Pemikiran Kritis Mahasiswa
- Presentation Accept
- Presentation and Personalization Management
- Presentation Brothers College, Cork
- Presentation client
- Presentation Connect
- Presentation Connection Endpoint
- Presentation Connection Endpoint Identifier
- Presentation Context Definition List
- Presentation Context Identifier
- Presentation Controller Mediator Entity Foundation
- Presentation Convent Kodaikanal
- Presentation copy
- Presentation Data Value
- Presentation Department
- Presentation Departments
- Présentation des Normes Européennes
- presentation drawing
- Presentation du Systeme de Planification et de Gestion de Frequence
- Presentation Element Parser, YACC
- Presentation Environment for Multimedia Objects
- Presentation File
- Presentation Function
- Présentation Générale Lex Persona
- presentation graphics
- presentation graphics program
- Facebook Share

Tools for the Patient Presentation
The formal patient presentation.
- Posing the Clinical Question
- Searching the Medical Literature for EBM
Sources & Further Reading
First Aid for the Wards
Lingard L, Haber RJ. Teaching and learning communications in medicine: a rhetorical approach . Academic Medicine. 74(5):507-510 1999 May.
Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format . Academic Medicine. 74(10):S124-S127.
The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) http://meded.ucsd.edu/clinicalmed/oral.htm
"Classically, the formal oral presentation is given in 7 minutes or less. Although it follows the same format as a written report, it is not simply regurgitation. A great presentation requires style as much as substance; your delivery must be succinct and smooth. No time should be wasted on superfluous information; one can read about such matters later in your admit note. Ideally, your presentation should be formulated so that your audience can anticipate your assessment and plan; that is, each piece of information should clue the listener into your thinking process and your most likely diagnosis." [ Le, et al, p. 15 ]
Types of Patient Presentations
New Patient
New patients get the traditional H&P with assessment and plan. Give the chief complaint and a brief and pertinent HPI. Next give important PMH, PSH, etc. The ROS is often left out, as anything important was in the HPI. The PE is reviewed. Only give pertinent positives and negatives. The assessment and plan should include what you think is wrong and, briefly, why. Then, state what you plan to do for the patient, including labs. Be sure to know why things are being done: you will be asked.
The follow-up presentation differs from the presentation of a new patient. It is an abridged presentation, perhaps referencing major patient issues that have been previously presented, but focusing on new information about these issues and/or what has changed. Give the patient’s name, age, date of admission, briefly review the present illness, physical examination and admitting diagnosis. Then report any new finding, laboratory tests, diagnostic procedures and changes in medications.
The attending physician will ask the patient’s permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may offer input or ask questions at any point. When presenting at bedside the student should try to involve the patient.
Preparing for the Presentation
There are four things you must consider before you do your oral presentation
- Occasion (setting and circumstances)
Ask yourself what do you want the presentation to do
- Present a new patient to your preceptor : the amount of detail will be determined by your preceptor. It is also likely to reflect your development and experience, with less detail being required as you progress.
- Present your patient at working or teaching rounds : the amount of detail will be determined by the customs of the group. The focus of the presentation will be influenced by the learning objectives of working responsibilities of the group.
- Request a consultant’s advice on a clinical problem : the presentation will be focused on the clinical question being posed to the consultant.
- Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
- Enlist cooperation required for patient care : a short presentation focusing on the impact your audience can have in addressing the patient’s issues.
Preparation
- Patient evaluation : history, physical examination, review of tests, studies, procedures, and consultants’ recommendations.
- Selected reading : reference texts; to build a foundational understanding.
- Literature search : for further elucidation of any key references from selected reading, and to bring your understanding up to date, since reference text information is typically three to seven years old.
- Write-up : for oral presentation, just succinct notes to serve as a reminder or reference, since you’re not going to be reading your presentation.
Knowledge (Be prepared to answer questions about the following)
- Pathophysiology
- Complications
- Differential diagnosis
- Course of conditions
- Diagnostic tests
- Medications
- Essential Evidence Plus
Template for Oral Presentations
Chief Complaint (CC)
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it. For ongoing care, give a one sentence recap of the history.
History of Present Illness (HPI)
This will be very similar to your written HPI. Present the most important problem first. If there is more than one problem, treat each separately. Present the information chronologically. Cover one system before going onto the next. Characterize the chief complaint – quality, severity, location, duration, progression, and include pertinent negatives. Items from the ROS that are unrelated to the present problem may be mentioned in passing unless you are doing a very formal presentation. When you do your first patient presentation you may be expected to go into detail. For ongoing care, present any new complaints.
Review of Systems (ROS)
Most of the ROS is incorporated at the end of the HPI. Items that are unrelated to the present problem may be briefly mentioned. For ongoing care, present only if new complaints.
Past Medical History (PMH)
Discuss other past medical history that bears directly on the current medical problem. For ongoing care, have the information available to respond to questions.
Past Surgical History
Provide names of procedures, approximate dates, indications, any relevant findings or complications, and pathology reports, if applicable. For ongoing care, have the information available to respond to questions.
Allergies/Medications
Present all current medications along with dosage, route and frequency. For the follow-up presentation just give any changes in medication. For ongoing care, note any changes.
Smoking and Alcohol (and any other substance abuse)
Note frequency and duration. For ongoing care, have the information available to respond to questions.
Social/Work History
Home, environment, work status and sexual history. For ongoing care, have the information available to respond to questions.
Family History Note particular family history of genetically based diseases. For ongoing care, have the information available to respond to questions.
Physical Exam/Labs/Other Tests
Include all significant abnormal findings and any normal findings that contribute to the diagnosis. Give a brief, general description of the patient including physical appearance. Then describe vital signs touching on each major system. Try to find out in advance how thorough you need to be for your presentation. There are times when you will be expected to give more detail on each physical finding, labs and other test results. For ongoing care, mention only further positive findings and relevant negative findings.
Assessment and Plan
Give a summary of the important aspects of the history, physical exam and formulate the differential diagnosis. Make sure to read up on the patient’s case by doing a search of the literature.
- Include only the most essential facts; but be ready to answer ANY questions about all aspects of your patient.
- Keep your presentation lively.
- Do not read the presentation!
- Expect your listeners to ask questions.
- Follow the order of the written case report.
- Keep in mind the limitation of your listeners.
- Beware of jumping back and forth between descriptions of separate problems.
- Use the presentation to build your case.
- Your reasoning process should help the listener consider a differential diagnosis.
- Present the patient as well as the illness .
- << Previous: Home
- Next: Posing the Clinical Question >>
- Last Updated: Jul 19, 2023 10:52 AM
- URL: https://rowanmed.libguides.com/tools
Basic Medical Terminology 1
Sep 11, 2014
1.08k likes | 2.68k Views
Basic Medical Terminology 1. Introduction. Medical words are used daily media doctors, nurses working life Examples arthritis hepatitis anemia Useful to learn medical terminology. Objectives. Enable you to understand the common medical terms
Share Presentation
- combining form
- combining vowel
- medical terminology
- word root vowel
- basic medical terminology 1

Presentation Transcript
Introduction • Medical words are used daily • media • doctors, nurses • working life • Examples • arthritis • hepatitis • anemia • Useful to learn medical terminology
Objectives • Enable you to understand the common medical terms • Allow you to explore and learn the vocabulary of the medical field • Equip you with knowledge useful for daily work in the health care setting
Lecture Schedule • Lecture 1 • Introduction • Word Structure and Analysis • Suffixes • Lecture 2 • Prefixes • Enlarging your medical vocabulary
Introduction to Medical Terminology
Introduction • Most medical terms come from • Greek language • diagnosis, surgery • Latin languages • anatomical names • Many sound mysterious • but can be easily worked out
Word Structure • All words have a word root • eg: trans/port ex/port • Compound words • words with 2 or more roots • eg: grand-father fire-fighter
Word Structure • Vowel • often added to a root word • allows formation of a compound word • makes pronunciation easier • Combining form • word root + vowel • eg: therm/o/meter micr/o/scope
Word Structure • Suffix • attached to root • eg: practition-er • Medical terms • like jigsaw puzzle • divided into several parts • Example • HEMATOLOGY • HEMAT /O/LOGY
Suffix Root (“study of”) (“blood”) Word Analysis • 1st step • look at end of the word • suffix • 2nd step • look at beginning • root word • gives meaning of term • 3rd step • combining vowel • usually consists of vowel “o” HEMAT/O/LOGY Combining vowel
Suffix Root Combining vowel (“study of”) (“blood”) Word Analysis HEMAT / O / LOGY • the study of blood
Root Suffix Root Electr/o/cardi/o/gram • suffix • “gram” - a record • 1st root • “electr” - electricity • 2nd root • “cardi” - heart • combining vowel • “o” -connects roots with suffix
Word Analysis Electrocardiogram • record of the electricity in the heart • combining form • combining vowel + root • eg: cardi/o • heart • eg: electr/o • electricity
Root Suffix Root Gastr/o/enter/o/logy • Suffix • logy • 1st combining form • gastr/o • 2nd combining form • enter/o • study of the stomach and intestines
Word Analysis • Gastr/o/scope • suffix scope • instrument to visually examine • combining form gastr/o • stomach • instrument to visually examine the stomach
Word Analysis • Gastr/ic • suffix • adjective: pertaining to • combining vowel is dropped when suffix begins with a vowel • root • stomach • pertaining to stomach
Word Analysis • Cardi/ac • suffix • adjective: pertaining to • combining vowel dropped • root • heart • pertaining to the heart
Word Analysis • Enter/itis • suffix • inflammation • combing vowel dropped • root • intestines • inflammation of the intestines
Suffixes • attached to the end of root words to further its meaning • 2 groups • those that describe diagnoses • describe condition of patient • those that describe procedures
Diagnostic Suffixes • -algia • pain • eg: neuralgia arthralgia • -itis • inflammation • eg: arthritis carditis
Diagnostic Suffixes • -ia • a state or condition • eg: bradycardia pneumonia • -osis • abnormal condition • eg: neurosis
Diagnostic Suffixes • -iasis • condition, formation of • presence of stone (lith-) • eg: nephrolithiasis • -genic • origin, producing • eg: neurogenic causes pathogenic bacteria
Diagnostic Suffixes • -emia • condition involving blood • eg: anemia septicemia, bacteremia • -megaly • enlargement • eg: acromegaly hepatomegaly, cardiomegaly
Diagnostic Suffixes • -oma • tumor, swelling • eg: breast adenoma • -oid • being like, resembling • eg: uterine fibroid • -lysis • break down, loosening • eg: hemolysis
Procedural Suffixes • describe medical procedures • looking into body parts • types of surgical repair • removal of body part • examples • -ectomy • -otomy • -scopy
Procedural Suffixes • -ectomy • excision of, removal of • may or may not remove entire organ • eg: tonsillectomy hepatectomy • -otomy • a surgical incision • eg: craniotomy, laparotomy
Procedural Suffixes • -centesis • surgical puncture with a needle • eg: amniocentesis thoracocentesis • -scopy • insertion of an instrument to visualize • eg: gastroscopy, cystoscopy
Procedural Suffixes • -plasty • surgical correction, plastic repair • eg: hip arthroplasty • -ostomy • operation to create opening (stoma) • eg: colostomy
Other Suffixes • do not fit into either category • -logy • study of • eg: biology cardiology • -form • shape • eg: deformed
Other Suffixes • -gram, -graph • a written record • eg: • electrocardiogram • polygraph machine • measures several parameters
Other Suffixes • -graphy • process of recording • eg: photography
Review • Root word • gives essential meaning of term • Suffix • word end • Combining vowel • connects root to suffix /other roots • Combining form • combination of root and combining vowel
TEST YOUR KNOWLEDGE 1. All words have a A. root B. vowel C. prefix
TEST YOUR KNOWLEDGE 2. The root in the medical term “tonsillitis” is A. itis B. sill C. tonsill 3. “Fasciotomy” is an example of a A. simple word B. compound word C. combining word
TEST YOUR KNOWLEDGE 4. When you analyze a medical term, begin at the A. beginning of the word B. middle of the word C. end of the word 5. Adding a vowel to a root results in a A. prefix B. combining form C. complex word
TEST YOUR KNOWLEDGE 6. Which of the following can be used to divide words into their word parts? A. / B. = C. … 7. Which of the following combinations do not need a combining vowel? A. dermat + itis B. micr + scopy C. dermat + logy
TEST YOUR KNOWLEDGE 8. Combining forms A. are always used to end a medical term B. are never connected to a suffix C. are never used to end a medical term 9. The word gastroduodenoscopy has A. 1 root B. 2 roots C. 3 roots
TEST YOUR KNOWLEDGE 10. In the word “ physiology”, the suffix is A. phy B. physio C. logy
Divide each of the following words into their component parts Word Root wordCombining Vowel Suffix Cardiologist Biology Mammogram Bronchoscopy Arthritis Inguinal Pneumonia Oncologist Cardiologist Biology Mamm o gram Bronch o scopy Arthr - itis Inguin -al Pneumon - ia Onc ologist
- More by User
Basic Terminology
Qualitative Non-numerical Based on direct observation Equipment not necessary Focus on time and space Examples: Rotation of femur during golf swing Adduction of humerus during freestyle swim. Quantitative Numerical Based on data collected Equipment necessary Focus on forces
1.13k views • 28 slides
Basic Terminology. EXPONENT. means. BASE. IMPORTANT EXAMPLES. Variable Expressions. This property is used to combine 2 or more exponential expressions with the SAME base. MULTIPLICATION PROPERTIES. PRODUCT OF POWERS. Write each product in expanded form, then rewrite in exponential form.
284 views • 11 slides
Medical Terminology: Basic Word Structure
Medical Terminology: Basic Word Structure. This tutorial has some nice use of audio, and the assessment is done well. The screen design is not so good, and the font is too large throughout. The use of cheesy clip art cost points. Overall it looks too much like a presentation.
965 views • 22 slides

Medical Terminology
Medical Terminology. Commonly used suffixes. COMMONLY USED SUFFIXES. Suffix Meaning - algia G. algos , pain.e.g arthralgia - ectomy G. ek -tome, cutting out. - itis G. suffix indicating inflammation. -al. Meaning pertaining to e.g neural
306 views • 6 slides
6. Medical Terminology. Introduction. Medical terminology is the language of health care. Medical terminology is much more concise than normal English for describing things of a medical nature. By understanding terms, components, even complex words, can be broken down.
808 views • 21 slides
Medical Terminology Assignment 1
Medical Terminology Assignment 1. Dr. Walid Daoud. I- In the space provided build combining forms for the following word roots. 1- mast (breast) ------------------- 2- hepat (liver) ------------------- 3- arthr (joint)
484 views • 9 slides
Medical Terminology. Objectives. Upon completion of this unit you will be able to: Identify and define the four word parts Identify and define a combining form Analyze and define medical terms Build medical terms for given definitions.
1.57k views • 46 slides

Medical Terminology. 外国语与国际交流学院 许 瑾.
1.05k views • 32 slides

Medical Terminology. Prefixes, Roots & Suffixes. Roots Prefixes Suffixes. Yellow – 70 Pink – 36 Blue – 25. Flash Cards. Help with Learning / Proven to Work! Easy to Use Color Coded for ease of Understanding. General Roots. Part 1. anter. Front. carcin. cancer. cry. Cold. cyan.
2.44k views • 152 slides

Medical Terminology. List 9. urethr/o. utethra (tube that carries urine from the bladder to the outside of the body). urethr/o. urethra (tube that carries urine from the bladder to the outside of the body) Urethra Urethral Pertaining to the urethra Urethritis
378 views • 27 slides
A Programmed Learning Approach to the Language of Health Care, 2 nd Edition. Medical Terminology. Chapter 2: Health Care Records. History and Physical (H&P). Document of medical history and findings from physical examination Includes:
641 views • 35 slides

Medical Terminology. Objectives. Identify basic medical abbreviations selected from a standard list Define prefixes, suffixes and word roots selected from a list of words Spell and pronounce medical terms correctly. Common Abbreviations Derived from Latin Terms.
498 views • 17 slides
Medical Terminology. List 11 Abbreviations Part 2. Hct. Hematocrit It is the percentage of blood volume that is occupied by red blood cells. It is normally about 47% for men and 42% for women. Hgb. Hemoglobin Hgb is the iron containing, oxygen transport protein in red blood cells. h.s.
498 views • 27 slides
Medical Terminology. Class #3. Medical Terminology. Do page one of your medical terminology worksheet. Take a break when you are finished. Prefixes – a word element at the beginning of the word to alter its meaning. A prefix can not stand alone; it must be combined with a root word.
1.01k views • 26 slides
Medical Terminology. The Immune system. Medical Terminology. Combining form/word root Meaning a den /o gland carcin /o cancerous; cancer - oma tumor
539 views • 9 slides
Medical Terminology. Circulatory System. Medical Terminology. Combining form Definition aden /o gland a ngi /o vessel a ort /o aorta
289 views • 6 slides
Medical Terminology. Anatomical Position. Standing erect, with ________ _________________________ Is the standard reference point in which all positions, movements, and planes are described. Anatomical Planes.
506 views • 38 slides
Medical Terminology. Senses. Medical Terminology. Word Parts : Meaning : blephar /o eyelid
261 views • 7 slides
Medical Terminology. Unit 5 Pathology, Otorhinolaryngology, and Prefixes dys-, brady-, tachy-, poly-, syn-. Cocc/i. Cocc/i (plural): spherically shaped family of bacteria. Coccus (singular) Coccos = Grain or seeds Bacteria types: Pneum/o/cocc/us Pneum/o/cocc/i
609 views • 37 slides
Medical Terminology. Introduction Mrs. Elizabeth Keele, RN. Chapter 1 Pages 1-4. Word Analysis. HEMATOLOGY HEMAT/O/LOGY Root Suffix (blood) (Study of) Combining Vowel. When you analyze a medical term, begin at the end of the word.
341 views • 20 slides
Medical Terminology. List 2. carcin/o R ★. cancer, cancerous Carcinoma carcinogen. Carcinoma ☤. Carcin / oma Carcin = cancer -oma = tumor or mass Tumor or mass of cancer. cephal/o R ★. Head Cephalic. Cephalic ☤. Cephal / ic Cephal = head -ic = pertaining to
727 views • 63 slides
Medical Terminology. Unit 15 Ophthalmology, Endocrinology, and Medical Specialties. Ophthalm/itis: Inflammation of the eye Ophthalm/ic: Pertaining to the eye Ophthalm/algia, Ophthalm/o/dynia: Pain in the eye Ophthalm/o/meter: Instrument for measuring the eye (curvature of the cornea).
1.11k views • 55 slides

IMAGES
VIDEO
COMMENTS
The oral presentation is a critically important skill for medical providers in communicating patient care wither other providers. It differs from a patient write-up in that it is shorter and more focused, providing what the listeners need to know rather than providing a comprehensive history that the write-up provides.
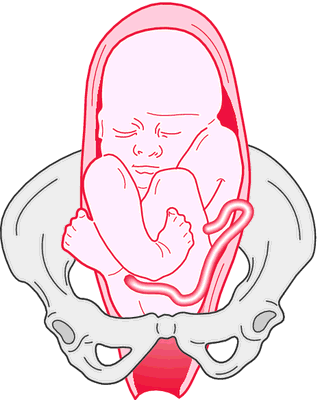
This definition of medical jargon appears to be a dictionary definition. Please rewrite it to present the subject from an encyclopedic point of view. (May 2023) In medicine, a presentation is the appearance in a patient of illness or disease—or signs or symptoms thereof—before a medical professional.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics. Note that there is an acceptable range of how oral presentations can be delivered.
presentation. (prĕz′ən-tā′shən, prē′zən-) n. Medicine. a. The position of the fetus in the uterus at birth with respect to the mouth of the uterus. b. A symptom or sign or a group of symptoms or signs that is evident during a medical examination: The patient's presentation was consistent with a viral illness. c.
A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Academic Medicine. 74(10):S124-S127. ... The attending physician will ask the patient's permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may ...
Enlist cooperation required for patient care: A short presentation focusing on the impact your audience can have in addressing the patient's issues. Preparation: Patient evaluation: history, physical examination, review of tests, studies, procedures, and consultants' recommendations. Selected reading: reference texts; to build a ...
How to Present a Patient. Opener. You should begin every oral presentation with a brief one-liner that contains the patient's name, age, relevant past medical history, and chief complaint. Remember that the chief complaint is why the patient sought medical care in his or her own words.
Slide 6. Here's an example of how each is used. The first word is cardiology. The word root is cardi (pronounced CARD-ee) which means heart. So our term cardiology means study of the heart. The second word example is tachycardia (pronounced tacky-CARD-ee-uh). The prefix is tachy (pronounced tacky), which means fast.
PPT in Medical commonly refers to Pain Pressure Threshold, which is a measure used to assess the sensitivity to pain and the level of pressure that elicits a pain response in individuals. It is a crucial parameter in pain management and research. Explore categories such as Medical and Healthcare for more information. 8.
Presentation Transcript. TEST YOUR KNOWLEDGE 1. All words have a A. root B. vowel C. prefix. TEST YOUR KNOWLEDGE 2. The root in the medical term "tonsillitis" is A. itis B. sill C. tonsill 3. "Fasciotomy" is an example of a A. simple word B. compound word C. combining word.